Authors: Soonman KWON and Eunkyoung KIM
Coronavirus disease 2019 (COVID-19) has disrupted all aspects of our global society and economies and progress towards universal health coverage (UHC), further worsening structural fragilities and deepening inequalities (1). Some countries that have designed their health systems for universality based on a whole system approach with a unified information platform and provider payments were better prepared and more resilient and performed better in responding to the pandemic.
- Benefits of investing in health system strengthening towards UHC
Investing in health systems and UHC, which ensures access to quality health services for all without financial hardship, contributes to improved health, a fundamental component of well-being and human capital development. Improved health contributes to fostering economic growth through higher productivity at all life stages (2). Progress towards UHC leads to financial protection for all regardless of the status of employment or residence, improving labour market mobility (3). Moreover, the health sector is a major source of employment, with multiplier effects on the wider economy, generating opportunities for creating formal jobs (4–6). UHC also contributes to poverty alleviation by providing financial protection and reducing impoverishment related to health expenditure (7,8). Public financing for UHC can contribute to improved efficiency, transparency and fiscal disciplines; given the magnitude and growth of the health sector, impacts of efficiency gains in the health sector on the overall government expenditure can be large (3,9). UHC with functioning health systems has the capacity for protecting a country’s economy from the impact of pandemics like COVID-19 (3,10,11). Sufficient funding and effective service delivery for pandemic preparedness and response as part of UHC (or progress towards UHC) reduce the risks of an outbreak, enable quick response and protect the vulnerable, increasing social stability and prosperity (3).
- UHC and health systems resilient to emergencies
To make health systems more resilient to shocks and crises, it is critical for governments to invest in core health system functions such as financing, service delivery and governance. Ensuring sufficient resources for health is necessary for basic infrastructure, human resources for health, and essential medicines, including vaccines; the overall level of health expenditure and the public sources of funding are important. Funding for public health services, including infection prevention and control (IPC), surveillance and information systems, is fundamental to ensure health systems are prepared for and responds to health emergencies (12). More importantly, funding should be made available for a quick and effective response to emergencies, requiring a supportive flexible public financial management (PFM) system (13). Moreover, it is essential to mitigate the potential risks of health system collapses through innovative ways of responding to health security issues and mobilizing private sector providers (13). Vulnerable groups who are even more impacted during crises need special attention (14). Multisectoral cooperation among the public and private sectors, all ministries and levels of government, and development partners is paramount to progress towards UHC as well as health system resilience and during pandemic response (3,15,16).
- COVID-19 pandemic and its impacts in Asia and the Pacific
As of 8 January 2021, more than 86.4 million confirmed COVID-19 cases and more than 1.8 million deaths have been reported. About 20% of global COVID-19 cases have been in Asia and the Pacific (17). Many countries have taken effective and proactive measures to contain the pandemic, such as non-pharmaceutical interventions (NPIs) including closing borders, schools, businesses and workplaces, restricting movement and gatherings, and conducting active surveillance, contact tracing and case management.
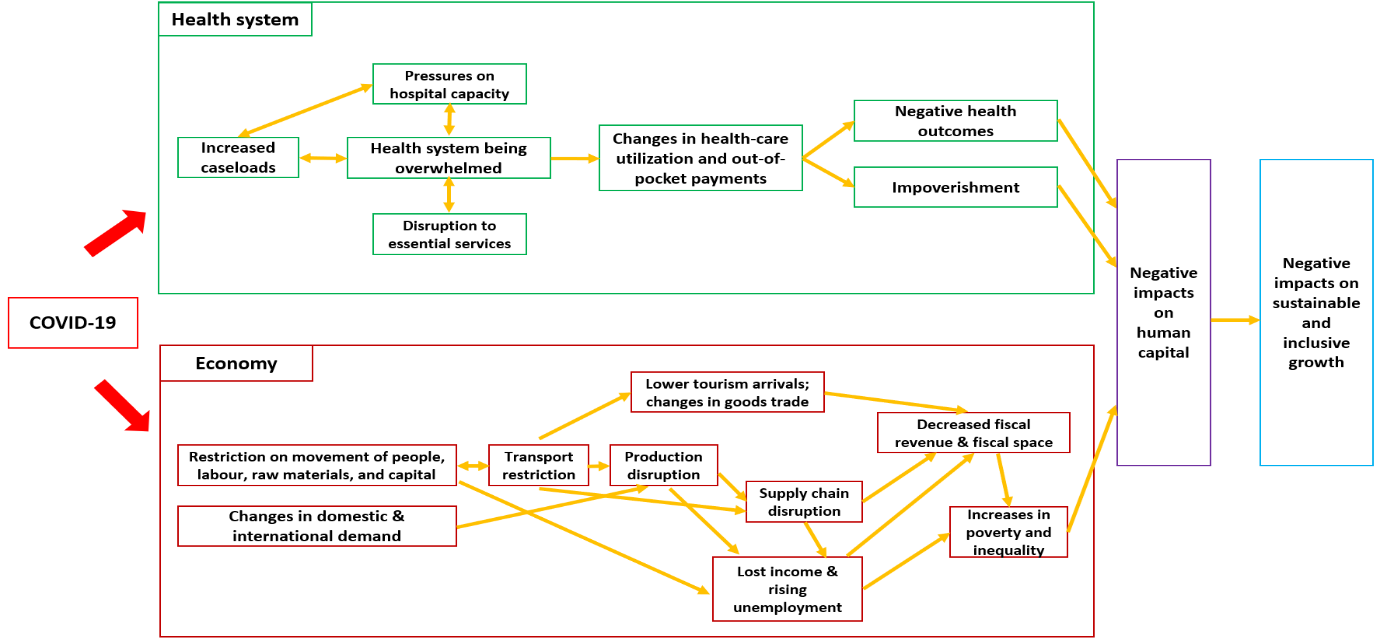
Impacts of COVID-19 on health systems and economies
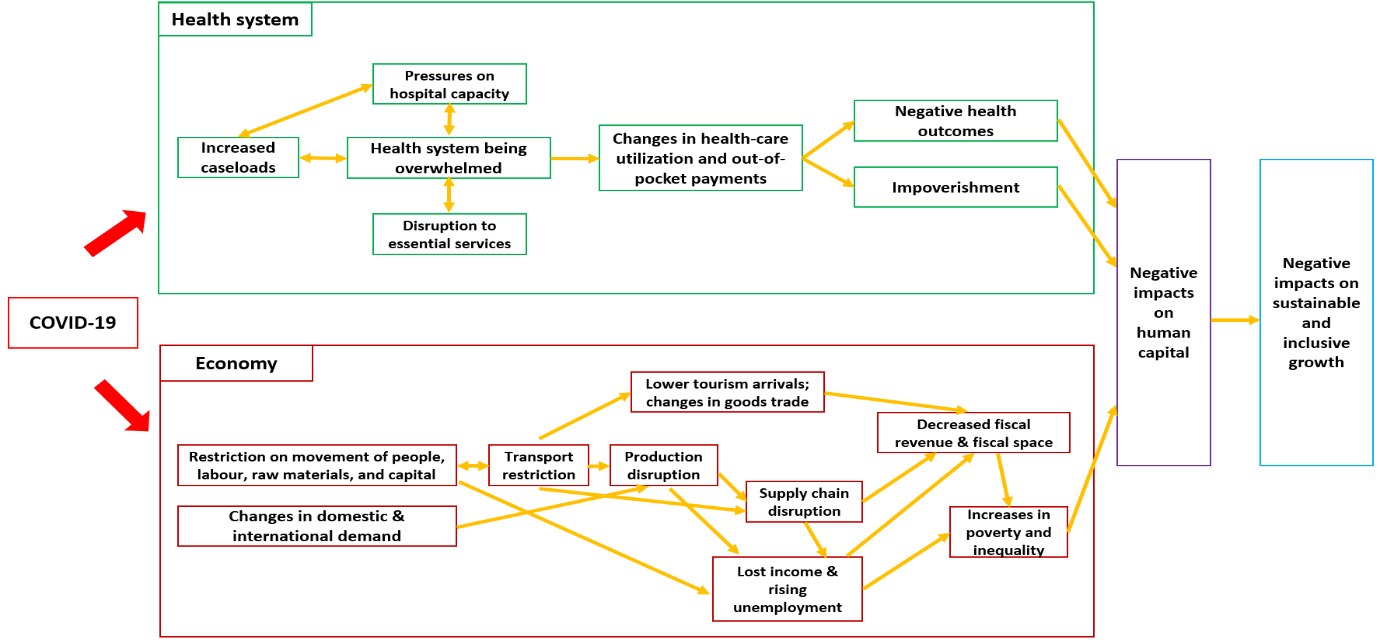
However, these containment measures have disrupted health systems and economies. Health systems are being overwhelmed by COVID-19 patients, while struggling to maintain access to essential health services (1). Preliminary evidence shows that essential services, such as immunization, maternal and child health, and noncommunicable diseases (NCDs), were partially or entirely disrupted (18). The COVID-19 pandemic and containment measures have also disrupted global supply chain and economic activities, affecting the economies’ production and leading to massive job and income losses (19,20). According to the International Monetary Fund, the global economy is projected to contract by 4.9% in 2020. Developing Asia’s economic growth is projected at 0.1% in 2020; growth is expected to contract in all subregions except East Asia (growth rate of 1.3%) (21). Based on estimates by the Asian Development Bank, the global economic impact of COVID-19 is projected to reach US$5.8 trillion (6.4% of global gross domestic product, or GDP) using a three-month scenario and US$8.8 trillion (9.7% of global GDP) in a six-month scenario. The economic impact on Asia and the Pacific could reach US$1.7 trillion (6.2% of regional GDP) and US$2.5 trillion (9.3% of regional GDP), respectively, accounting for 30% of the overall decline in global GDP (19). The pandemic will have an impact on poverty and inequalities. Impacts from increases in poverty and decreases in income, especially among the poor and vulnerable, would be harmful to health, education, nutrition and living conditions, seriously affecting human capital development (14).
4. Sustainable financing for UHC and health system resilience
The current crisis has tested the features of sustainable financing of health systems and their pandemic preparedness. Resilience in revenue raising, pooling, purchasing and service delivery has proven to be key in responding to such crises. Countries need to evaluate the existing arrangements to rebuild and prepare for future crises as well to improve efficiency and equity in the access to health care.
Revenue raising
Tax funding is more efficient than contribution-based systems to enhance pandemic preparedness, in particular when contributory schemes do not cover an entire population or when it is based on multiple separate pools. Compared with contribution-based financing, government funding has a higher capacity to swiftly implement countercyclical fiscal measures and adjust entitlements to ensure access to care during a pandemic. Job losses and the inability to pay contributions have negative effects on financial protection of the unemployed as well as on the fiscal stability of the contributory financing system. To overcome the decrease and unpredictability in the revenue generation during a crisis, a government’s willingness and flexible PFM rules and processes are necessary to facilitate swift reprioritization and reallocation of public funds and emergency injection of additional funds to the health sector.
Pooling
A single pool can effectively steer the development, investment and implementation of preparedness and coordinate the response across all relevant stakeholders. Even in a single pool of contributory financing, coordination between contributions and government budget is important during a pandemic response. In a system of multiple pools, harmonization of entitlements and service coverage across pools, risk equalization, and uniform information systems can strengthen health system preparedness and resilience during a pandemic (22).
Purchasing
Service coverage
Health financing should provide comprehensive coverage and access to essential medicines and health services, including preparedness for outbreaks and pandemics. Key public health functions, tests, diagnostics and personal protective equipment, among others related to a pandemic response, should be available as an entitlement without financial barriers (12). A PFM system needs to include special arrangements and procedures that allow fast and transparent flexibility to reallocate funds or purchase goods and services to adjust to changing needs in the response to a pandemic, including for the poor and vulnerable. Purchasing arrangements need to be designed to ensure minimum disruption during a pandemic in the provision of essential health care, such as vaccination, mental health, NCD, and reproductive, maternal and child health services.
In Asia and the Pacific, COVID-19 services in most countries have been funded by government budgets or public insurance systems. In China, Indonesia, Malaysia, Mongolia and Viet Nam, for example, government budgets were employed for both regular and emergency purposes. Funding from (public) health insurance systems have contributed to COVID-19 services in India, Japan, the Republic of Korea and the Philippines, among others. Australia, Cambodia, China, Japan, the Lao People’s Democratic Republic, Malaysia, Mongolia, the Philippines, the Republic of Korea, Singapore, Thailand and Viet Nam offer testing and treatment of COVID-19 free of charge.
Payment system for providers
Quick and flexible purchasing in times of a pandemic includes making available additional public resources to front-line service providers in a timely manner. Resilient health systems have quickly adjusted PFM rules and procedures as well as fiscal arrangements, such as advance payments or direct budget transfers, that aimed at accelerating the release of funds to providers. The Philippine Health Insurance Corporation, or PhilHealth, under the interim reimbursement mechanism released funds paid to health-care facilities equivalent to three months’ worth of claims based on historical data, which will be accounted for in future claims (23). Temporary compensation for providers for unexpected changes in cash flow is needed to enable smooth, effective adaptation.
Purchasing arrangement for private providers
A surge of patients during a pandemic requires mobilizing both public and private providers for a whole-of-country approach. Based on quality and performance, having in place a contracting system for private providers would be fundamental for pandemic preparedness. Incentive and payment systems for private (and public) providers as well as legislation, accreditation and regulation for the quality of health-care providers constitute pandemic preparedness. A PFM system needs to include contracting arrangements with private providers during a pandemic if such rules are not in place. By June 2020 private providers in most countries of Asia and the Pacific had already been mobilized to support the COVID-19 response actions to some extent, including testing, consultations, dispensing of outpatient medicines, intensive care, hospital admissions and quarantine, and self-isolation measures. Payment rates for private providers have been adjusted to offer incentives for more accessible COVID‑19 services (24).
Adaptable PFM
Many countries in Asia and the Pacific have reallocated existing public resources through virements or initiated supplementary budgets. The quick access and use of savings in line ministries’ respective budgets can support faster response and action on account of policy priorities, as was done in India and the Philippines, for example. Australia, New Zealand and the Philippines have program-based budgets that feature an adaptable PFM system where government budgets can be reprogrammed with ease to move funds to where they are most needed. Having a fast PFM authorization process allows the rapid release of public funds to health providers and can potentially maximize the budgetary space for health in emergencies. Mechanisms to concentrate on payments to policy priorities must be in place. Governments with centralized payment mechanisms through the national treasury are in a better position to ensure payment prioritization. Decentralized payment mechanisms will have to be informed by local-level prioritization; in this setting, clear guidelines from the central authorities on prioritization is important. Within limits, delegating some payment authorities to line ministries and spending units may also be considered for faster budget execution and release of funds.
Service delivery
Pandemic preparedness calls for special wards and hospitals for the treatment of patients, and the health system requires flexibility in infrastructure, logistics and human resources to respond to a pandemic (13). Setting up a patient triage system and sending mild patients to non-hospital facilities can free up hospital beds for patients with severe illness, and the coordinated continuum of care can reduce mortality. During the COVID-19 pandemic, resilient health systems quickly expanded local innovations to adapt to the needs and surge capacity. Digital health has shown to improve access to care during a pandemic in many countries. For digital health to succeed, adequate payments and incentives for both providers and patients, as well as a system to ensure quality, safety and privacy, should be considered.
5. Conclusion
The COVID-19 pandemic has exposed the intrinsic value of health and resilience of the health sector, the importance of sufficient investment in health, and the interconnectedness of health and the economy. Learning from the COVID-19 crisis, countries need to take this opportunity to build back better through pro-poor policies, sustainable economic policies and greater investment in public services, including building resilient health systems for UHC and health security.
Acknowledgements
This work was part of the background paper on UHC and COVID-19 preparedness and response in Asia and the Pacific for the health ministers’ meeting and the joint health and finance ministers’ symposium in September 2020, funded by the WHO Regional Office for the Western Pacific and the Asian Development Bank.
We appreciate valuable inputs and feedback from Peter Cowley, Tomas Roubal, Ding Wang, Ronald Tamangan (WHO Regional Office for the Western Pacific), Valeria De Oliveira Cruz, Tsolmongerel Tsilaajav (WHO Regional Office for South-East Asia), Joseph Kutzin (WHO headquarters), Eduardo Banzon and Patrick Osewe (Asian Development Bank) on an earlier version of the manuscript.
References
1. A UN framework for the immediate socio-economic response to COVID-19. New York (NY): United Nations; April 2020.
2. The Human Capital Project. Washington (DC): World Bank; 2018.
3. High-performance health financing for universal health coverage. Washington (DC): World Bank; 2019.
4. Improving employment and working conditions in health services. Geneva: International Labour Organization; 2017.
5. Health employment and economic growth: an evidence base. Geneva: World Health Organization; 2017.
6. Working for health and growth: investing in the health workforce. Geneva: World Health Organization; 2016.
7. Global monitoring report on financial protection in health 2019. Geneva: World Health Organization and International Bank for Reconstruction and Development/The World Bank; 2020.
8. Wagstaff A, Flores G, Smitz M-F, Hsu J, Chepynoga K, Eozenou P. Progress on impoverishing health spending in 122 countries: a retrospective observational study. The Lancet Global Health. 2018;6:e180–e92.
9. Cashin C, Bloom D, Sparkes S, Barroy H, Kutzin J, O’Dougherty S. Aligning public financial management and health financing: sustaining progress toward universal health coverage. Health Financing Working Paper No. 4. Geneva: World Health Organization; 2017.
10. Towards a global action plan for healthy lives and well-being for all: uniting to accelerate progress towards the health-related SDGs. Geneva: World Health Organization; 2018.
11. von Schirnding Y. Health and sustainable development: can we rise to the challenge? The Lancet. 2002;360:632–7.
12. Kutzin J. Priorities for the health financing response to COVID-19 [web story]. P4H Social Health Protection Network; 2 April 2020 (https://p4h.world/en/who-priorities-health-financing-response-covid19, accessed 31 July).
13. Maintaining essential health services: operational guidance for the COVID-19 context. Geneva: World Health Organization; 2020.
14. Loayza NV. Costs and trade-offs in the fight against the COVID-19 pandemic: a developing country perspective. Washington (DC): World Bank; 2020.
15. Thomas S, Sagan A, Larkin J, Cylus J, Figueras J, Karanikolos M. Strengthening health systems resilience: key concepts and strategies. Brussels: European Observatory on Health Systems and Policies; 2020.
16. Kwon S. COVID-19: lessons from South Korea [news story]. Health Systems Global; 31 March 2020 (https://healthsystemsglobal.org/news/covid-19-lessons-from-south-korea/, accessed 28 July 2020).
17. WHO coronavirus disease (COVID-19) dashboard. Geneva: World Health Organization; 2021 (https://covid19.who.int/?gclid=CjwKCAjwm_P5BRAhEiwAwRzSO5LuKjw-KoAyPyq0viccKIsmTbe9rUtNesIBWjomUCmukTccg8oSOBoCZpoQAvD_BwE, accessed 8 January 2021).
18. COVID-19 and NCDs: preliminary results of rapid assessment of service delivery for NCDs during the COVID-19 pandemic. Geneva: World Health Organization; 2020.
19. An updated assessment of the economic impact of COVID-19 [ADB Briefs]. Manila: Asian Development Bank; 2020.
20. The social and economic impact of COVID-19 in the Asia-Pacific Region. Bangkok: United Nations Development Programme; 2020.
21. World Economic Outlook Update. Washington (DC): International Monetary Fund; 2020.
22. Mathauer I, Saksena P, Kutzin J. Pooling arrangements in health financing systems: a proposed classification. Int. J. Equity Health. 2019;18:198.
23. PhilHealth Circular No. 2020-0007 Guidelines on the provisions of effective privileges to those affected by a fortuitous event. Manila: PhilHealth; 2020.
24. Tsilaajav T. Purchasing health services to respond to COVID-19: how to invovle and contract private sector providers in the South-East Asia Region? [web story]. P4H Social Health Protection Network; 29 June 2020 (https://p4h.world/index.php/fr/node/9320, accessed 14 August 2020).