It’s a goal that has challenged many a health ministry: how to free up significant resources for health services by increasing health budget execution.
Late last year, health sector practitioners from eight countries (Bangladesh, Ghana, Kenya, Lao PDR, Liberia, Malaysia, Nigeria, and Peru) met to tackle the issue head-on as participants in the Joint Learning Network Health Budget Execution Learning Exchange, an initiative led by the USAID Local Health System Sustainability Project (LHSS) in collaboration with the Joint Learning Network for Universal Health Coverage (JLN). They made meaningful progress.
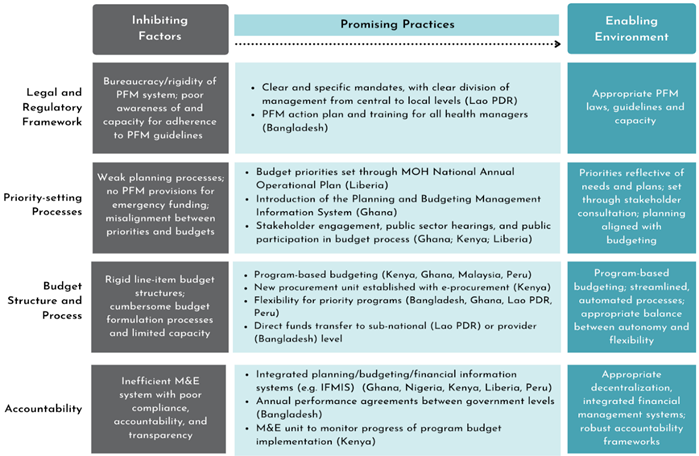
The learning exchange participants first identified the key factors that affect health budget execution. These factors, they agreed, are 1) a country’s legal and regulatory framework, 2) its priority-setting processes, 3) its budget structure and process, and 4) its mechanisms for accountability. (See the first blog in this series). Then they shared their experiences in implementing small but important practices to get past bottlenecks in these four areas and move from an inhibiting to an enabling environment for health budget execution (Figure 1).
Promising practices to build an enabling environment for good health budget execution
Legal and regulatory framework. The release of budgets to health care providers is a form of provider payment, and the legal and regulatory framework for how providers are paid matters. Paying providers based on outputs and service delivery objectives is important for linking spending to priorities, but rigid public financial management systems can inhibit this. Participants from Peru shared that the budget execution rules of the national health insurance program, Seguro Integral de Salud, allow flexibility in how providers are paid to deliver services. Seguro Integral de Salud makes pre-payments to health facilities at the beginning of the year, and the payments are reconciled at the end of the year based on the volume of services delivered.
Priority-setting processes. In many countries, poor budget execution can be traced back to weak priority-setting processes within the health sector. Participants from Ghana, Kenya, and Liberia shared how they engaged stakeholders in priority-setting for the budget process to ensure that priorities reflect the voices of a wide range of stakeholders. In Kenya, well-organized public hearings are carried out at the county level for public participation in the budget process. In Liberia, stakeholder consultations include patients; health facility staff; Ministry of Health, district, and county health teams; and non-health stakeholders including the Ministry of Finance and legislature.
Budget structure and process. Participants from Bangladesh and Lao PDR shared how streamlining the flow of funds from the central to the subnational level has reduced the layers of approval and helped get funds to service providers more directly. In Lao PDR, strengthening the role of subnational stakeholders in budget planning, and strengthening communications channels and processes between central and provincial levels, helped to better execute health budgets.
Accountability. In Ghana and Bangladesh, integrated financial management information systems have helped improve budget formulation, execution, and accountability in real time. Liberia shared how its annual public expenditure review process has enabled public financial management improvements, while Nigeria described how the Fiscal Responsibility Act has led to more transparent, accountable, and prudent management of the country’s resources.
Figure 1. Pathways Towards an Enabling Health Budget Execution Environment
The promising practices shared by countries provide concrete examples of how Ministry of Health practitioners have proactively improved their budget execution while accounting for factors unique to the health sector. These unique factors that affect health budget execution were discussed recently during the 5th Meeting of the Montreux Collaborative on fiscal space, public financial management, and health financing. They include the vulnerability of health spending to health emergencies that are difficult to budget for; uncertainty about health utilization; the larger proportion of a health budget that is variable compared to budgets in other sectors; and different financing arrangements that exist in the health sector (e.g., whether financing is centralized at the line ministry, via a separate purchasing agency, or decentralized).
During the Montreux meetings, colleagues from the World Health Organization and the World Bank introduced their work to develop a framework and tool that will identify policy solutions in a coordinated manner between health and finance stakeholders. These policy-level solutions, combined with information on how countries have implemented promising practices through the LHSS-JLN learning exchange, will provide richer guidance to help countries improve their health budget execution.
Stay tuned for the next blog in this series to learn how Kenya, Lao PDR, and Malaysia improved their budget structures and processes for better health budget execution, in particular through direct transfers of funds to subnational level entities and program-based budgeting.
About the author:
Heather Viola is a program officer at R4D and manages the LHSS-JLN Health Budget Execution Learning Exchange.
Additional contributors:
Karishmah Bhuwanee is a Senior Associate at Abt Associates and leads the LHSS Health Budget Execution Activity.
Cheryl Cashin is a managing director at R4D and the lead author of the joint R4D-WHO publication, “Aligning Public Financial Management and Health Financing.”
Sarah Insanally is a Senior Associate at Abt Associates and is a senior technical contributor to the LHSS Health Budget Execution Activity.
Nivetha Kannan is a program associate at R4D and a member of the technical facilitation team for the LHSS-JLN Health Budget Execution Learning Exchange.
Aparna Kollipara is a health financing expert and a member of the technical facilitation team for the LHSS-JLN Health Budget Execution Learning Exchange.
Miriam Omolo is a health financing expert and country facilitator for LHSS-JLN Health Budget Execution Learning Exchange. She also serves as Executive Director at The African Policy Research Institute.


