Nicole Fraser, Adanna Chukwuma, Marianna Koshkakaryan, Lusine Yengibaryan, Xiaohui Hou, Tommy Wilkinson, Christina Meyer
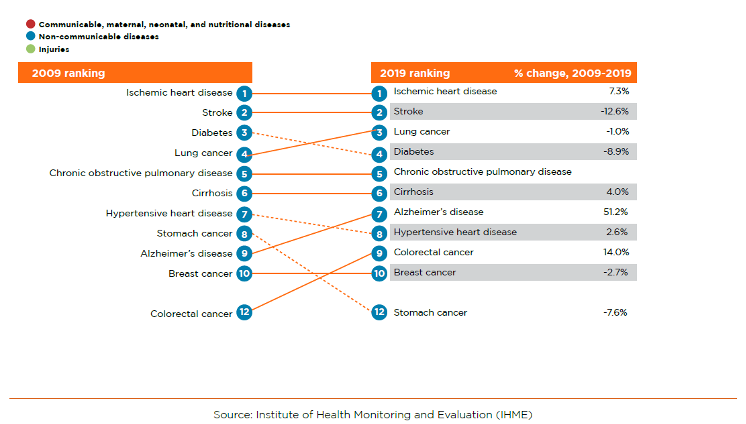
When Armenia introduced its first Basic Benefits Package (BBP) in 1997, the average life expectancy at birth was 70 years and the under-five mortality rate was 35 deaths per 1,000 live births. Over the past twenty years, the under-five mortality rate has fallen to 12 deaths per 1,000 live births and life expectancy has risen to 75 years. At the same time, the proportion of the population aged 65 years and above has risen from 6 to 12 percent, and non-communicable diseases (NCDs), including cardiovascular diseases (CVDs) and cancers, have become the predominant causes of death and disability (Figure 1). Compared to other countries with similar social and demographic indicators, Armenia has a higher age-standardized rate of disability-adjusted life years per 100,000 people, due to ischemic heart diseases, stroke, and diabetes.
The BBP as the main instrument for universal access to essential health services
Access to high quality health care is essential for preventing and managing NCDs. However, while 100 percent of pregnant women receive antenatal care and birth attendance from a skilled provider, essential services for NCDs are underutilized. For example, less than 25 percent of adults have been screened for diabetes mellitus, and only 44 percent have been screened for hypertension. These health care utilization patterns reflect in part differential coverage for different services and population groups within the BBP.
The BBP, financed through the national budget, provides the Armenian population with universal access to emergency and primary health care, excluding most outpatient medicines. The government also funds hospital care and expensive diagnostic services for 30 percent of Armenians, including some state employees, low-income families, and socially vulnerable groups. Hence, for the majority of the population, out-of-pocket (OOP) payments are the predominant source of financing for care, introducing barriers to utilization. Groups with expanded coverage through the BBP have 36 percent higher rates of outpatient care utilization. About 85 percent of total health spending is paid by OOP, far above the average of 31 percent in upper-middle-income countries or 30 percent in the European region.
The government has periodically reviewed the BBP by changing the scope of services, population groups covered by the benefits, and reimbursement rates. However, budgeting and political considerations are the main considerations for these changes, rather than the disease burden and health service priorities. Some services in the package are also reimbursed at levels that are below the cost of delivery, owing in part to the low levels of public health financing, incentivizing the undersupply of these services by providers and demand for informal payments. Armenia cannot finance all services for the entire population. However, to make progress towards UHC, given public health financing constraints, the process of revising the BBP should consider key technical criteria, including the disease burden, health service utilization rates, and the need for financial protection.
Exploring options for a more inclusive and higher impact BBP
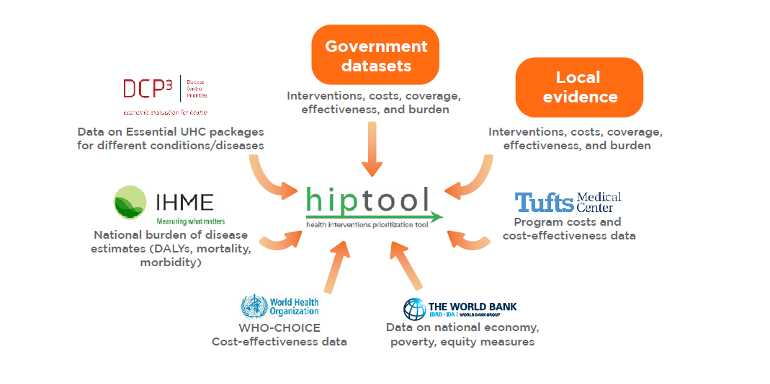
Jointly with the Armenia Ministry of Health, the World Bank conducted an assessment using the Health Intervention Prioritization tool (HIPtool) to identify potential modifications to the BBP that can facilitate improvements in population health. The HIPtool uses a model-based algorithm to identify optimal resource allocations that maximize health outcomes, subject to the public health spending, disease burden, intervention coverage and effectiveness, cost-effectiveness, and societal value for equity and financial protection (Figure 2). The tool provides analytical outputs that can inform stakeholder discussions on future changes to the BBP that respond to emerging health needs.
The study team investigated three different scenarios to explore the hypothetical impact of a re-designed BBP:
In Scenario 1, we optimized spending within the 2019 budget, allowing for a maximum increase of 10 percent intervention coverage, to understand how the BBP services could be re-prioritized in the short-term.
In Scenario 2, we compared the optimized 2019 budget allocations with a hypothetical budget that was 40 percent higher than the current budget, to explore the additional health impact of increased public health financing.
Scenario 3 compared a model with increased weighting for cost-effectiveness, relative to equity and financial risk protection, with another model with equal weights for these factors.
Implications for getting more value-for-money from the BBP
1. Increase allocations to high-impact interventions: Optimizing the resource allocations to services within the BBP and the 2019 public health budget could have averted an additional 30,000 DALYs (Figure 3). Consistent with the country’s disease burden, the cardiovascular package of services received the most funding in both the 2019 and the optimized budget scenarios. However, we also identified the need for higher allocations to cost-effective interventions for musculoskeletal and cancer care that could address a considerable burden of disease.
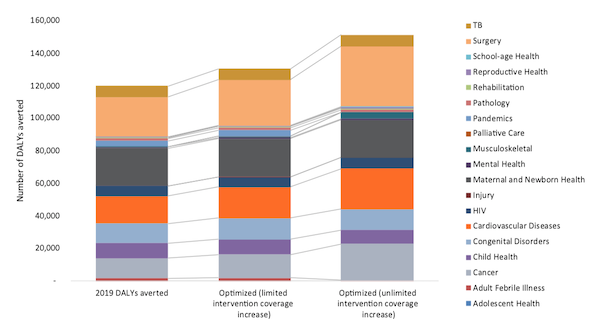
2. Increase public health financing: Increasing public health financing by 40 percent would avert an additional 15,000 DALYs, allocating additional financing to CVDs, surgery, mental health, palliative care, rehabilitation, and pandemic management. Optimizing spending within the lower budget reduced allocations for critical interventions, including palliative care, mental health, maternal and newborn health. This analysis illustrated how the limited public spending on health restricts investments in cost-effective interventions that would otherwise target prioritized population groups.
3. Pooling public health financing: In the model, we pooled resources for vertical programs supported by the government and development partners, with finances for health services in general. The optimization demonstrated that there are opportunities to improve health spending efficiency through reallocations between vertical programs and other services. The transition from donor to state funding for health offers national stakeholders an increased autonomy over spending allocations to reap these efficiency gains.
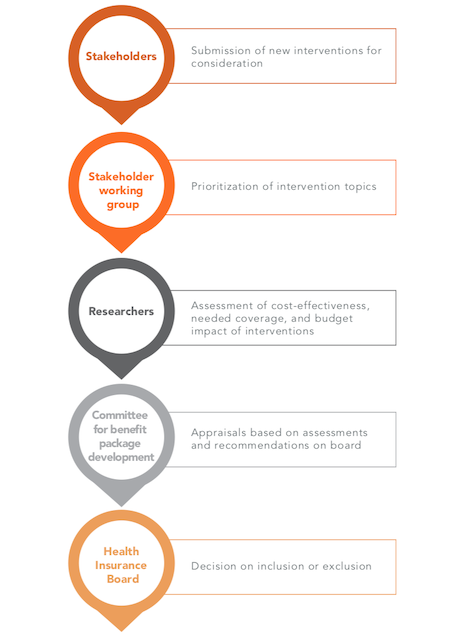
4. Introducing systematic health technology assessments (HTA): This analysis illustrates the benefits of introducing a systematic process for reviewing the BBP, that accounts for critical technical criteria. Drawing on successful experiences in other countries, these assessments should be complemented by stakeholder consultations and should be encoded in legal documents (Figure 4). To this end, there is an ongoing private sector effort to build capacity for HTA, for medicines and health services, led by the Armenian Association of Specialists in Evidence-Based Medicine, the Armenian ETL Pharmacovigilance Center, and the Dutch HTA Development Platform. This may be an entry point for revisiting the process of revising the BBP in Armenia.
Conclusion
The results of the analysis were disseminated in a national UHC event in February 2021 attended by stakeholders from the Ministries of Health, Finance, and Economy, State Health Agency, National Institute of Health, National Center for Disease Control, and National Institute of Labor and Social Research. This was followed up with a workshop for key technical personnel in April 2021 on how to use the HIPtool software and parametrized Armenia model, embedded in wider reflections on what criteria and principles countries can use in benefits package design.
This allocative efficiency analysis is an illustration of how mathematical optimization can support decision making on Armenia’s future BBP, using an open-source tool. The HIPtool enables users to model different scenarios based on the disease burden, cost-effectiveness, total budget envelope, and societal value for equity and financial protection. Explicit analysis of value-for money in health care, as well as equity and financial risk protection will gain new urgency in the post-COVID-19 era. While the path to UHC will vary from country to country, national health benefit packages which are grounded in evidence will play a critical role in facilitating universal access to high-quality health care.
Read the full report here.


