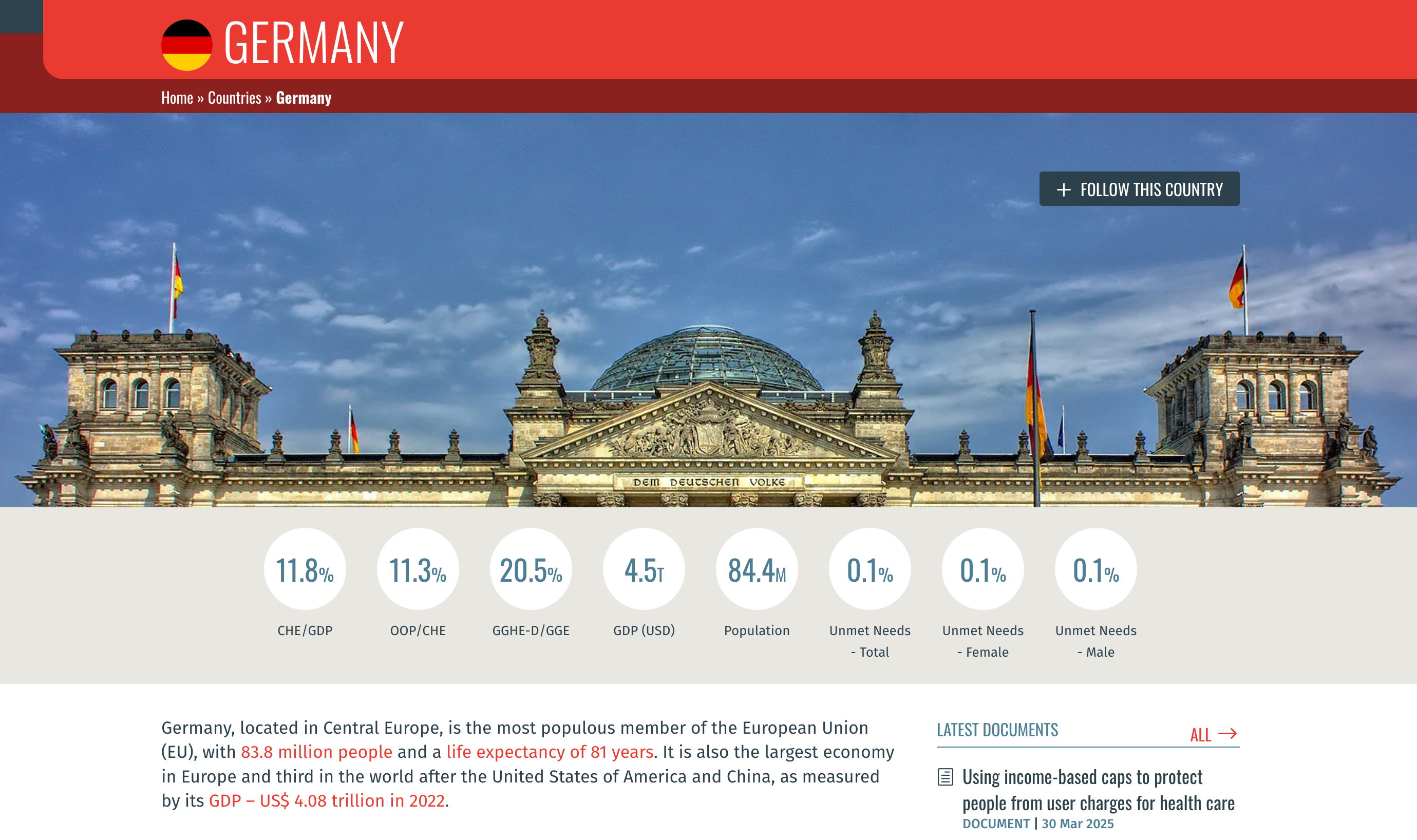
Germany has one of the lowest rates of unmet needs in Europe, with the difference in insurance coverage between income groups being less than one-fourth of a percentage point. Government health expenditures represent more than 20% of government expenditures, which is the fourth highest in the so-called WHO Europe Region in 2022.[1]
Germany’s health financing (HF) system, which is largely based on its mandatory health insurance system, comprises both statutory health insurance (SHI) and private health insurance (PHI).[2] It is built on the social insurance model established in 1883 under Otto von Bismarck[3] (chancellor of Germany at that time) that still stands today as a model of an insurance-based system advancing universal health coverage.
SHI covers about 89% of the population.[4] The following extract from Germany: Health Care & Long-Term Care Systems, published by the European Commission, lists the services covered by SHI.
SHI covers preventive services, inpatient and outpatient hospital care, physician services, mental health care, dental care, optometry, physical therapy, prescription drugs, medical aids, rehabilitation, hospice and palliative care, pregnancy care, maternal leave and sick leave compensation.
SHI operates with self-governing sickness funds (96 in 2023). The sickness funds collect contributions and send them to a central “reallocation pool”, the Gesundheitsfonds (in English, Health Fund), which reallocates the funds back, based on risk-adjusted criteria.[5] SHI contributions are calculated as a percentage of income, with supplementary premiums added by individual sickness funds when necessary.[6]
The following excerpt from Germany: Health System Summary 2022, published by the European Observatory on Health Systems and Policies, explains Germany’s health system governance.
Health system governance in the country is complex and decentralized: it is divided between the federal and state levels, and corporatist bodies of self-governance. While the federal level sets the overall legal framework, state governments are responsible for hospital planning and public health services, and for example, took leading roles in implementing measures to respond to the COVID-19 pandemic. However, most decision-making power within the SHI system is delegated to corporatist bodies (such as associations of providers and sickness funds). The public health, ambulatory and inpatient, and long-term care sectors in the health care system are subject to different legislation and thus are separated in terms of organization, financing and reimbursement.
[1] Global Health Expenditure Database, World Health Organization (choose country)
[2] Blümel, Miriam, et al. “Germany: Health System Review” Health Systems in Transition, vol. 22, no. 6, 2020, p. xxii.
[3] Ibid, p. 14.
[4] Blümel, Miriam, et al. “Germany: Health System Summary 2024” European Observatory on Health Systems and Policy, 2024, p. 5.
[5] Blümel, Miriam, et al. “Germany: Health System Summary 2022” European Observatory on Health Systems and Policies, 2022, p. 4.
[6] Blümel, Miriam, et al. “Germany: Health System Review” .” Health Systems in Transition, vol. 22, no. 6, 2020, p. xxiv.
[7] Ibid pp. xxiii-xxiv.
Key features of the German social health protection and health financing systems
TIMELINE – Germany’s SHP reforms from 1883 to 2025
Hospital Care Improvement Act
New hospital funding models and transformation fund.
Digitalization Acceleration Act
Nationwide e-prescriptions and electronic health records.
Statutory Health Insurance Financial Stabilization Act
Financial reforms in all areas of statutory insurance
Patient Data Protection Act
Legal framework for ePA and digital health data protection.
Digital Healthcare Act
Improve Healthcare Provision through Digitalisation and Innovation
Appointment Service and Care Act
Patients will get faster doctor appointments, with improved health insurance benefits and better care.
Statutory Health Insurance Contribution Relief Law
Equalized employer-employee split of supplementary statutory health insurance contributions.
Healthcare Strengthening Act
Act to strengthen health promotion and prevention.
Statutory Health Insurance Competition Strengthening Act
It includes mandatory coverage for everyone by 2009
Statutory Health Insurance Modernization Act
Reform the German healthcare system from a cost point of view
Pharmaceutical Budget Replacement Act
Replaced drug budgets with reference pricing.
Risk Structure Compensation Reform Act
Overhauled risk equalization among sickness funds.
Long-Term Care Insurance Act
Compulsory long-term care insurance introduced.
Health Care Structure Act
Most comprehensive reform of statutory health insurance since 1945
Health Care Reform Act
Global hospital budgets and drug reference pricing.
Hospital Financing Act
New federal hospital planning and financing mechanisms.
Imperial Insurance Code, Sickness Insurance
Expanded coverage to more workers and dependents.
Health Insurance Act
First compulsory sickness insurance for some workers.