Somalia’s health care system has been profoundly affected by decades of conflict and governance challenges,[1] leading to a fragmented and underfunded health sector. Nearly 50% of current health expenditure (CHE) comes from international sources, including nongovernmental organizations (NGOs) and United Nations agencies. The shift to federalism in 2012 aimed to improve governance, with overlapping responsibilities having further complicated the health financing landscape. The Federal Government of Somalia (FGS) now faces considerable challenges in mobilizing domestic resources for health to build a cohesive health system and associated policy framework.
Barriers to sustainable health financing
Somalia’s health financing is characterized by several critical barriers.
- Limited government revenue generation: The FGS has struggled both to generate sufficient domestic revenue and to dedicate it for health due to a weak tax base and ongoing security concerns. Consequently, government expenditure on health remains low, estimated at just 1.3% of total government spending in 2019.
- High out-of-pocket expenditures: No out-of-pocket spending or CHE data are available, but almost half of all households (48%) report finance health expenses using their own income despite low income levels, increasing their risk of experiencing catastrophic health spending.
- Fragmented private sector: While the private health care sector could account for 60% of CHE, it is largely unregulated and concentrated in urban areas, creating equity concerns and leaving rural populations underserved.
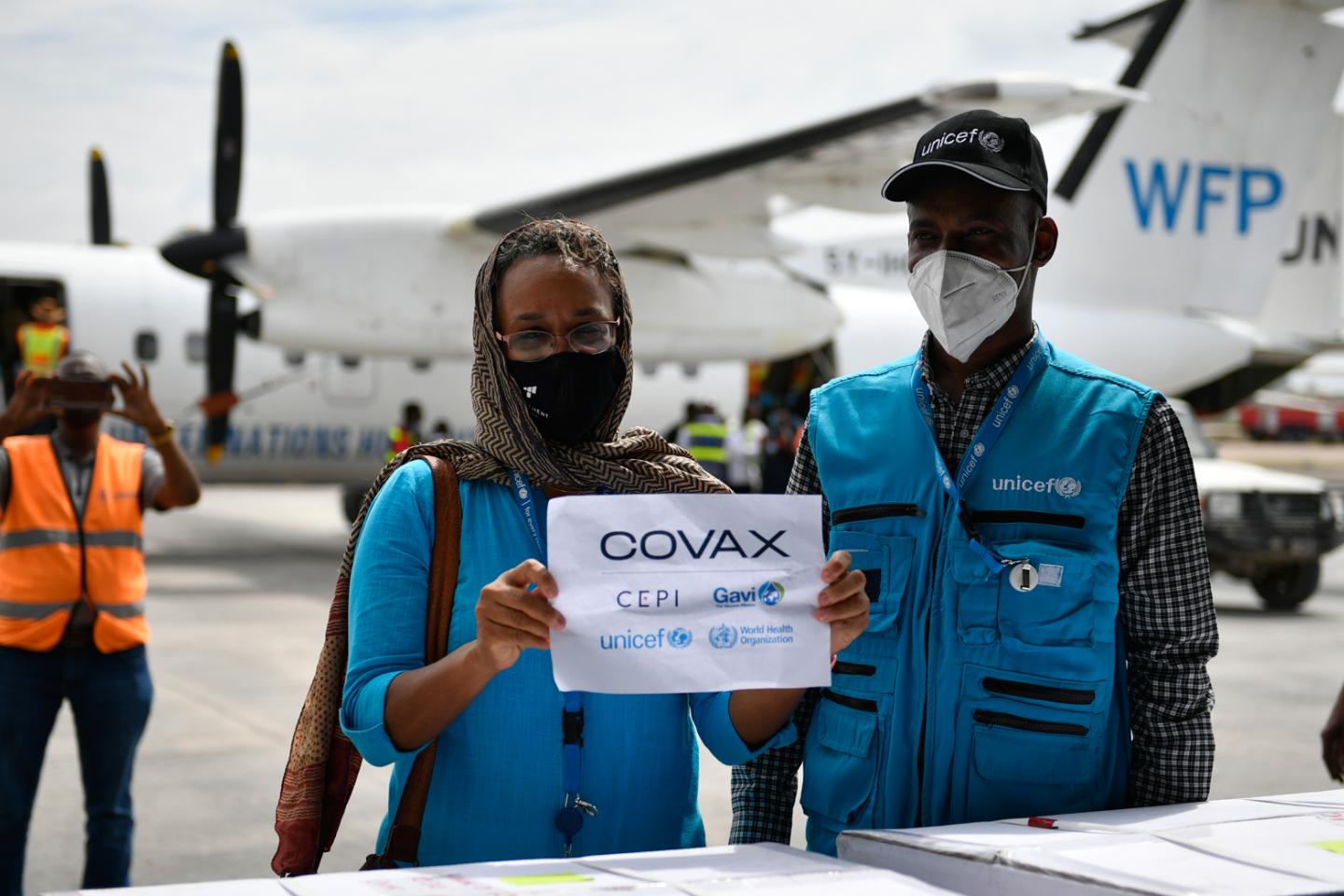
- Dependence on donor aid: In recent years, external aid has been substantial, with figures reaching approximately US$ 137 million in 2019. However, this funding often aligns with donor priorities rather than the expressed needs of the Somali health authorities.
Health financing reforms for universal health coverage
To advance universal health coverage, Somalia could implement reforms that address existing barriers.
- Strengthening domestic resource mobilization: Having recognized the importance of reducing dependency on donor funding, the government is exploring ways to increase health budget allocations through improved tax collection and innovative financing mechanisms.
- Capacity building for evidence-based health planning: Investments in health information systems and data collection are essential to evidence-based health financing decisions.
- Enhancing public-private partnerships: Leveraging the strengths of both public and private sectors is an option that could potentially improve service delivery and financing.
- Strategic partnerships with donors: Somalia’s government is also focusing on aligning donor contributions with national health priorities, aiming to shift from short-term, project-based funding to more sustainable, long-term investments.
References
[1] Ministry of Health, Federal Republic of Somalia, Investment Case for the Somali Health, Sector 2022–2027