Written by Eunkyoung Kim and Tomas Roubal
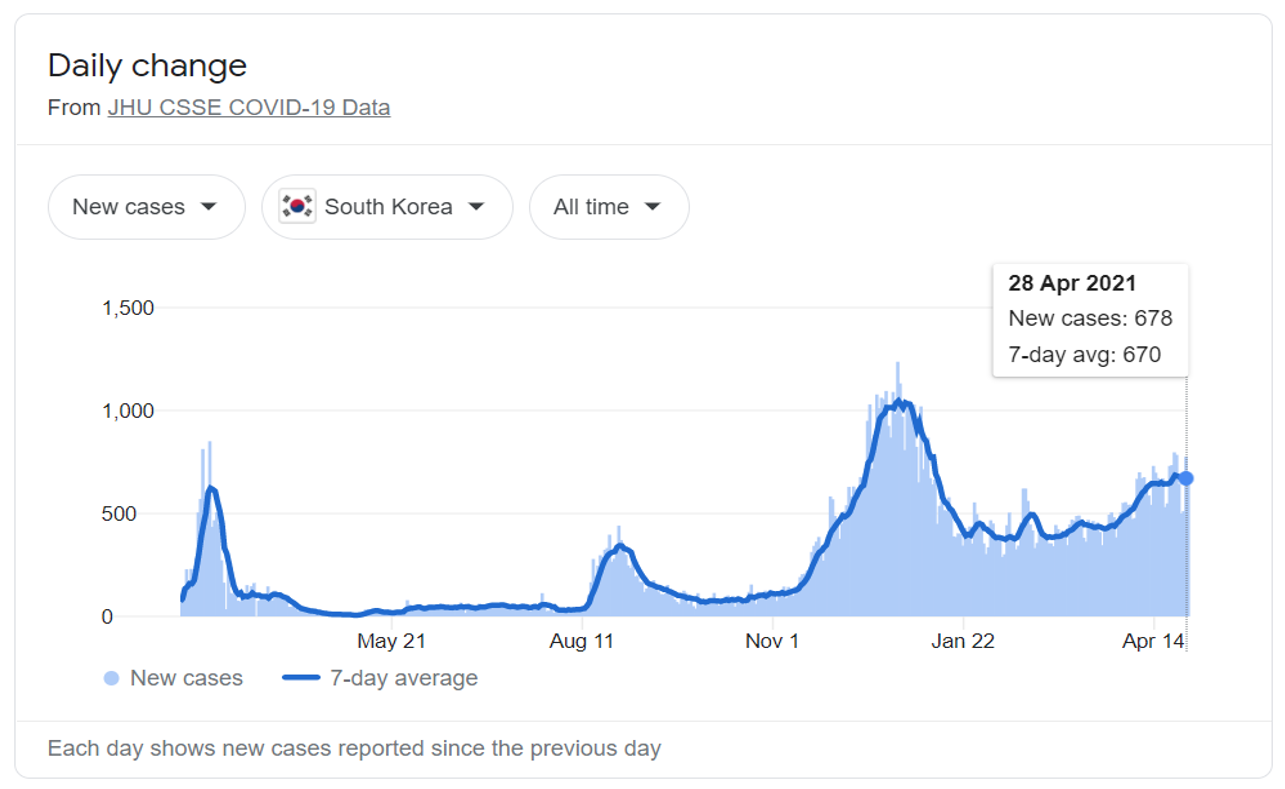
The Republic of Korea (ROK) has been regarded as one of successful countries in their response to coronavirus disease 2019 (COVID-19). As of 28 April 2021, ROK has reported 120,673 cumulative confirmed COVID-19 cases and 1,821 deaths since the first confirmed case on 20 January 2020; recently, a seven-day-average new cases per day were 670 (Figure 1).
From the outset, the government has taken proactive and strategic measures to contain the spread of COVID-19. This includes non-pharmaceutical interventions (NPIs), such as school closure, teleworking, closure of high-risk venues (e.g., religious facilities, indoor sports and entertainment facilities), social distancing measures (e.g., keeping spaces between people, recommending to avoid gathering in groups), and personal hygiene (e.g., wearing a mask, handwashing, coughing etiquette), without border closure (except Hubei, China) and lockdowns; active surveillance & case detection, and case management through test, tracing, and treatment activities. Implementing NPIs has contributed to enabling the government to strengthen preparedness and readiness for the COVID-19 response capacity. However, the implementation of NPIs impacted patients’ perception of health seeking, patterns of health care utilization, and access to health services. The growing backlog of health services deferred may lead to challenges in the health sector to meet unmet health needs in the future.
In Korea, the number of COVID-19 patients has not overwhelmed the capacity of the health system. The government has made efforts to maintain essential health service delivery through establishing effective patient flow, such as triage and targeted referral of COVID-19 and non-COVID-19 patients. In addition, telemedicine and prescription without visit was temporarily allowed to improve access to care and reduce potential infection during outpatient visits in vulnerable facilities including health facilities and nursing homes from the end of February 2020.
As a result, disruptions to essential health services have not been observed in Korea, but according to recent data, significant changes in health care utilization were found. It is important for policy makers to understand causes of such changes, which health facilities and which population groups were significantly impacted, and how much medical expenditure was impacted to make decisions on health policies for better and fairer health systems and for preparedness and response to a future pandemic.
Impacts of COVID-19 on health care in the Republic of Korea in 2020
Based on the Korean National Health Insurance (NHI) Statistics from the Health Insurance Review and Assessment service (HIRA), key messages were found by comparing data for January-September 2020 with data for January-September 2019 as follows.
- Decreased health utilization and increased medical expenditure in 2020
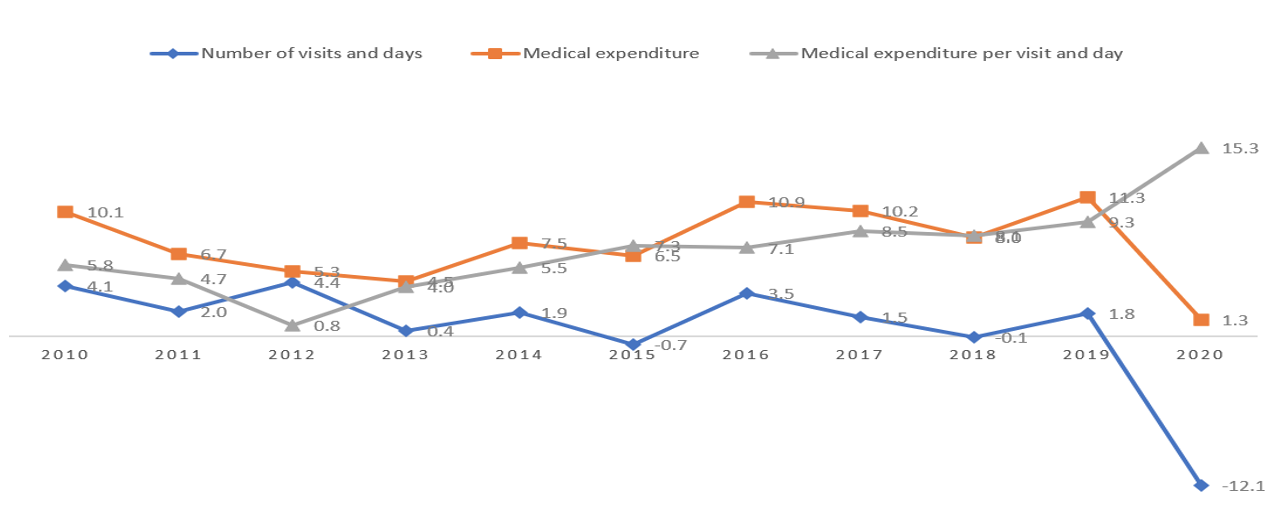
Overall, decreased health utilization and increased medical expenditure were found in Korea during the COVID-19 pandemic in 2020. The number of total health care utilization (including outpatient and inpatient care) has been decreased by 12.11%, which was the largest decline over a decade; the number of outpatient visits was largely declined by 12.9% compared to that of inpatient days (by 4.6%). Medical expenditure for the insured services has been only slightly increased by 1.3%, although this was the smallest increase rate over a decade; medical expenditures on inpatient care and outpatient care have increased by 2.8% and by 0.4%, respectively. However, the increase rate of medical expenditure per visit and day was the highest over a decade (increase rate of 15.26%), which was two and a half times higher than the average increase rate of 6.11% from 2010 to 2019; medical expenditure per visit and day on outpatient care has increased significantly by 15.26%, while that of inpatient care has increased by 7.78% (Figure 2).
- Changes in health care utilization
Health service utilization was decreased across almost all population groups (by age and sex); females (by 12.35%), children and adolescents (by 44.89% for the aged 0-9 years old; by 29.51% for the aged 10-19 years old), and young working population (by 12.7% for the aged 30-39 years old) decreased their utilization of healthcare services, particularly for outpatient care, leading to lower expenditure by the National Health Insurance (NHI) for those groups.
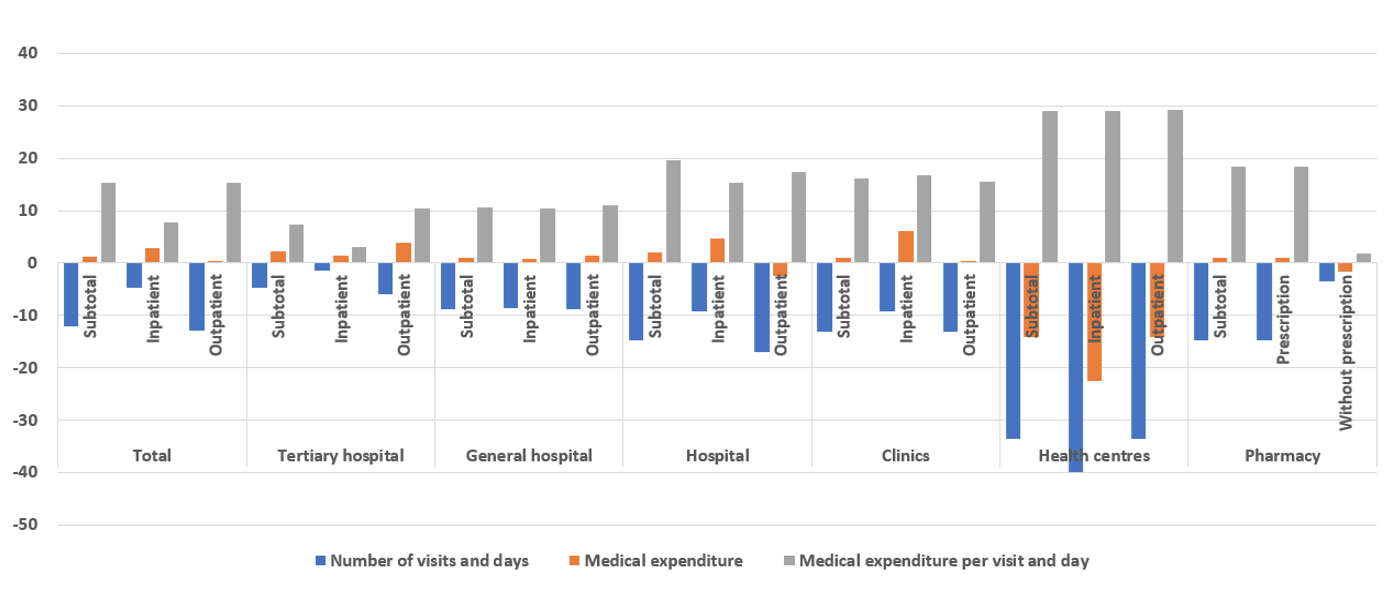
The number of outpatient visits significantly decreased (by 12.9%) compared to the drop of inpatient days (by 4.6%). Utilization in health centres dropped by one third (33.5%), and hospitals and clinics also saw large decreases in the number of patients (decreased by 14.7%, and 13.1%, respectively) (Figure 3). The ministry of Health and Welfare and local governments intentionally reduced the function of health centres on delivery of health services, re-focusing them towards tracing and testing as part of the COVID-19 response; health centers played a key part in the COVID-19 response, although they have relatively limited human resource.
Changes in utilization at hospitals and clinics might stem from four broad areas: i) changes in health seeking behavior due to personal perception (e.g., fear of cross-infection at the point of care among people); ii) changes in the burden of diseases (e.g., reduced flu cases and injuries); and iii) changes in the health system, entitlements or health financing not linked to COVID-19.
Impact of COVID-19 on health seeking behavior
• The number of utilization of almost all health facilities and pharmacies was declined compared to the same period in the previous year. According to the 2020 survey on patient experiences of health care utilization over the period from July 2019 to June 2020 conducted by the ministry of Health and Welfare, the share of people who worried about fear of cross-infection at the point of care has increased by 8.7 percentage points for outpatient care and 9.6 percentage points for inpatient care (14.7% for outpatient care and 18.1% for inpatient care in 2020). Thus, this would imply that fear of cross-infection has affected health seeking behavior, leading to avoidance of health care utilization among people during the COVID-19 pandemic.
Changes in the burden of diseases
• COVID-19 mostly affected clinics that provide outpatient care, which accounted for about 34% in the total health services utilization. Among clinics, utilization of pediatrics and ear/nose/throat clinics were significantly decreased by 44.9% and 29.8%, respectively. The number of patients with acute respiratory diseases in outpatient care was significantly decreased (acute bronchitis by 47.1%; acute sinusitis by 43.4%; acute tonsilitis by 40.5%; acute upper respiratory infection by 38.4%; flu by 34.8%), which are ones of common diseases covered by pediatrics and ear/nose/throat clinics. This also holds the same for inpatient care utilization; the number of patients with acute respiratory diseases in inpatient care was largely decreased (acute bronchitis by 55.2%; acute tonsilitis by 47.3%; pneumonia by 46.7%; influenza by 31.8%).
• The number of patients with depressive episodes and anxiety disorders have been increased by 6.5% and 4.5% amid the overall decrease of utilization in other areas; the number of visits to treat these diseases was increased by 9.7% and 7.4%, respectively. It is likely that the implementation of NPIs, its prolonged duration of the COVID-19 pandemic and containment measures in the response, the negative impact of COVID-19 on the economy and societies have affected the increases in stress levels among people, leading to the increased incidences of mental health problems such as depression, other anxiety disorders, and sleep disorder.
Government health policy actions to expand benefit packages including teleconsultation
• Even during the COVID-19 response, the government has managed to ambitiously expand benefit package based on the current government’s initiative of expanding benefit package in 2018-2022, including coverage of various ultrasound services, magnetic resonance imaging, and other 566 tests and services in Sep 2020. The government also temporarily introduced teleconsultation in the benefit package from 24 February 2020. The increases in medical expenditure in obstetrics (by 22.4%), urology (by 13.6%), ophthalmology (by 6.3%), and internal medicine (by 2.8%) clinics, and their relatively smaller decrease in the rates of utilization compared to those of other clinics can be partially explained by these policies.
- Changes in medical expenditure
With declines in health care use, medical expenditure on average was increased in 2020, particularly for tertiary hospitals (by 2.3%), hospitals (2%), general hospitals (1.1%), and clinics (by 0.9%). Moreover, medical expenditure per visit and day has significantly increased by 15.26%; among the major health facilities accounting for large shares in the utilization and medical expenditure, hospitals had the highest increase rate of 19.65% for medical expenditure per visit and day, followed by clinics (16.08%), general hospitals (10.71%), and tertiary hospitals (7.33%).
It seems that increased medical expenditure in Korea during the COVID-19 pandemic was a consequence of a series of intentional policy decisions in the COVID-19 response as well as a set of the existing policies and characteristics of the health system. There are several pathways how the COVID-19 pandemic led to changes in cost and health expenditure, including: i) increased intensity of inpatient services; ii) increased costs of care (e.g., PPE, infection prevention and control-IPC, pharmaceutical prescribing patterns); iii) additional services included with increased fees (e.g. teleconsultation); and iv) financial incentives and adaptation to public financial management, cash flow and provider payment methods.
Increased intensity of inpatient care
• Firstly, it has something to do with the characteristics of patients (e.g., severity of health conditions), affecting the level of intensity of care provided. Hospitals, general hospitals, and tertiary hospitals provide intensive care for COVID-19 patients with severe and critical conditions and other patients with severe diseases who need hospitalization, leading to increased medical expenditure due to intensive care for hospitalized patients. These high-level health facilities also have better infrastructures for innovative service delivery, and the majority of services provided in tertiary care hospitals were high-tech services and treatment. In addition, the levels of fees for services are higher in these hospitals than other health facilities such as clinics.
Increased cost of care
• High-level health facilities might also have maintained the level of medical expenditure covered by NHI through provider-induced services (e.g., prescribing unnecessary diagnostic procedures, unnecessary follow-up visits). And they might have increased costs of care through PPE, IPC, prescribing medications for longer periods and so on.
Additional services included with increased fees (e.g. teleconsultation)
• Consultation and prescription via telephone (teleconsultation) were temporarily introduced with some limited conditions from 24 February 2020. Since 8 May 2020, clinics have been allowed to receive an additional fee of teleconsultation (30% of the normal consultation fee), fully covered by NHI, which is added to the normal consultation fee for consultation and prescription via telephone; teleconsultation is more expensive than face to face consultation from a provider’s perspective.
Financial incentives and adaptation to public financial management, cash flow and provider payment methods
• The increase in medical expenditure may imply that the government made efforts to improve resilience and sustainability in the health system through flexible public financial management systems. To ensure maintaining cash flow to health care providers, the government shortened days of the reimbursement process from 22 to 10 days based on the National Insurance Enforcement Rule 21. For advance payment, 90~100% of the monthly average insurance benefit claim cost (for the same period in the previous year) were given to health facilities with financial difficulty related to COVID-19 in advance.
Conclusion
Although the Republic of Korea has reported relatively low number of COVID-19 cases and implemented minimum levels of NPIs, the COVID-19 pandemic has led to significant changes in health care utilization and medical expenditure in 2020. It is too early to conclude whether the decrease in utilization is associated with unmet need or the decreased use of unnecessary care. Therefore, continuous monitoring on health care utilization and medical expenditure and its impact on the health status in the future should be called for.
Acknowledgement
We appreciate valuable inputs and feedback from Peter Cowley, Ding Wang, Yeri Kim (WHO Regional Office for the Western Pacific), Ke Xu, Inke Mathauer, Joseph Kutzin, Susan Sparkes (WHO headquarters), and Soonman Kwon (School of Public Health, Seoul National University; Korea Health Industry Development Institute) on an earlier version of the manuscript.


