Health Policy and Systems Research (HPSR) is vital for creating robust, evidence-based health policies, improving health system performance, and ultimately enhancing the well-being of populations. However, domestic financing challenges for HPSR can pose significant obstacles to advancing research initiatives. Addressing these challenges requires strategic and sustainable commitment from the government and other stakeholders to allocate adequate resources and invest in long-term research capacity and infrastructure.
Domestic Funding Challenges:
A Health System StrA Health System Strengthening Accelerator supported pilot sought to identify the challenges faced by HPSR institutions (HPSRIs) in Asia and develop a preliminary framework responsive to those challenges, which can support HPSRIs to assess funding opportunities and promote domestic financing for HPSR in Southeast Asia. The work is co-led by the P4H Network and the Alliance for Health Policy and Systems Research with Seoul National University (SNU) as an implementing partner. engthening Accelerator supported pilot sought to identify the challenges faced by HPSR institutions (HPSRIs) in Asia and develop a preliminary framework responsive to those challenges, which can support HPSRIs to assess funding opportunities and promote domestic financing for HPSR in Southeast Asia. The work is co-led by the P4H Network and the Alliance for Health Policy and Systems Research with Seoul National University (SNU) as an implementing partner.
From October 2022 to September 2023, the SUN team, led by Professor Soonman Kwon conducted a mixed-methods study in two Southeast Asian Countries – Thailand and Vietnam – to understand the landscape of HPSRIs in the region, the respective research environments, and funding allocations for HPSR.
The SNU team, in partnership with the P4H and Alliance, developed an initial conceptual framework to assess HPSR funding, which they presented to experts in Vietnam and Thailand for further feedback. While the original incorporated profile aspects of the funder and HPSRI, field interviews highlighted the need to add a function that properly addresses how regulations, legislation, and other system-level policies shape how HPSR and HPSRIs evolve. These items are represented by “institutionalization.” The final conceptual framework incorporated six key aspects of domestic funding for HSPR to be assessed – theme, institutionalization, funder, HPSRI (funding recipients), performance, and core values. The “Institutionalization” item was added to the initial framework.
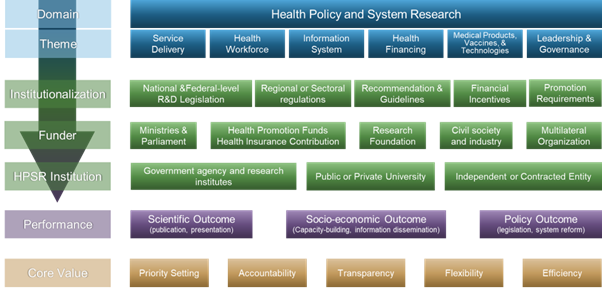
Figure 1: Adjusted Conceptual Framework to assess domestic funding for HPSR in Asia
Final Framework to assess domestic financing for HPSR in Southeast Asia
The research revealed HPSRIs in Thailand and Vietnam face challenges with low levels of funding, absence of long-term funding, fragmentation and duplication of funding distribution, the often complicated and non-universal definition of HPSR, and limited domestic capacity for HPSR were all significant challenges for HPSRIs:
- Financing: Funding for HPSR is still relatively small compared to other health services researchers, such as clinical and biomedical research. As of 2023, a majority of funding for HPSR still comes from international donors.
- Independence: Most HPSRs in Southeast Asian countries were implemented by public institutions or government agencies. This suggests autonomy in research is limited as HPSR is often implemented to support specific legislation rather than conducted independently.
- Fragmentation: In both countries, duplication and fragmentation remain challenging. The fragmentation in funding for HPSR partly originated from a lack of a universal definition for HPSR, making having a stand-alone budget difficult.
“The rapid growth in government funding that an HPSRI managed expanded its organizational role and its dependency on the government to some extent.”
HPSRI Respondent
Thailand
Despite these limitations, the team found remarkable developments in HPSR and its funding, from which other Southeast Asian countries can draw important lessons. In Thailand, establishing several public health institutes and funding bodies supported by legislative reforms led to an HPSR environment that includes public research institutions, R&D funding bodies, universities, and private research institutions in a relatively short period. In Vietnam, establishing the Health Strategy and Policy Institute (HPSI), a government research unit, promoted the value of HPSR within the country. To date, HPSI is the primary implementer of HPSR in the country.
The framework is not final. It needs to be tested, developed further, and adapted for different country -contexts to accurately capture the landscape of HPSR, the funding available, and unique health systems mechanisms or needs. Still, it can be used to support systems thinkers to articulate the current state of HPSR and its funding, along with the limitations and barriers to funding In Asia. We hope to continue refining this framework to provide additional insight into how HPSR is developing in the region and how HPSRIs navigate these systems to provide evidence and translate evidence for policymakers and other key stakeholders.


