Malaysia’s public healthcare is plagued by understaffing, low morale, overcrowding, and stagnant reform. Budget 2026 plans to absorb contract doctors, boost spending, strengthen public-private partnerships, roll out tech-driven workforce mapping, and build inclusive governance for systemic change.
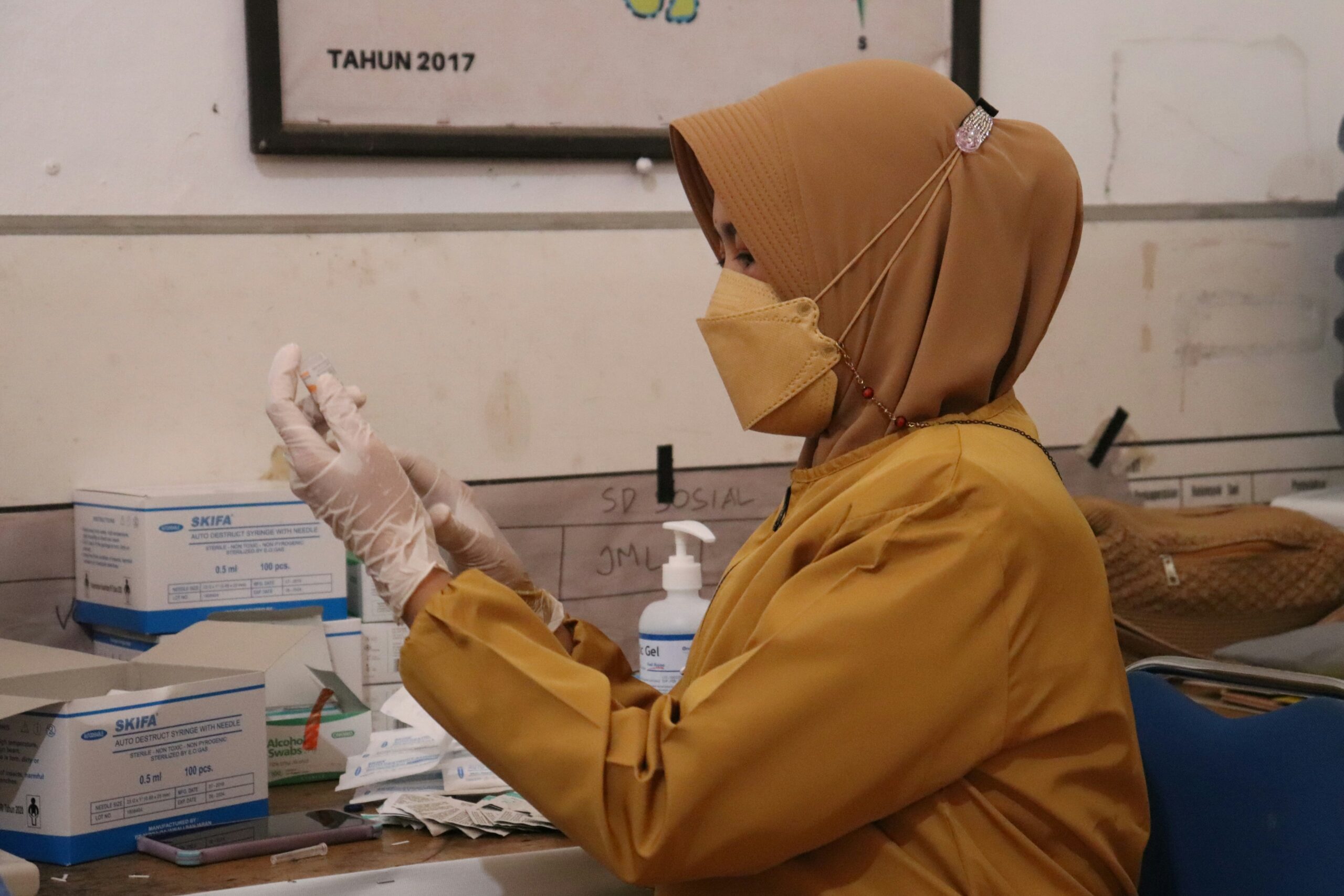
Malaysia’s public healthcare system, still reeling from post-pandemic stress, faces entrenched structural issues: a high attrition rate among healthcare workers (HCWs), low morale, and chronic overcrowding. Policies such as the contract doctor system and lack of permanent positions have driven many skilled professionals to other sectors or abroad. Severe understaffing and unsustainable workloads have further eroded morale, while overcrowded hospitals leave patients waiting over a day in emergency wards or months for surgery. Ill-conceived initiatives like the Rakan KKM programme and incomplete reforms such as the Diagnosis-Related Group (DRG) mechanism have compounded frustration among professionals. Meanwhile, stagnant consultation fees for private general practitioners (GPs) and limited public-private integration have alienated the primary care sector.
Budget 2026 presents a turning point to confront these long-standing problems. The Malaysian Medical Association (MMA) has proposed reforms under a People, Process, and Technology (PPT) framework to strengthen sustainability. Under “People,” it urges absorbing all contract doctors into permanent roles, raising on-call allowances, and fostering fair career pathways to retain talent. “Process” reforms include better manpower distribution, inspired by industries like aviation, and transparent HR systems such as the Pertukaran Suka Sama Suka (P3S) scheme, aimed at flexible staff transfers. However, bureaucratic inertia has stalled its progress. Under “Technology,” the rollout of an AI-driven national dashboard for workforce mapping could provide data-based transparency and reduce maldistribution across regions.
The MMA and other stakeholders call for raising public healthcare spending to 5 percent of GDP, up from 2.4 percent, recognizing healthcare as an investment in national resilience. This includes increasing public facility registration fees—excluding the poorest (B40)—to fund maintenance, and empowering an inclusive reform council comprising the Ministry of Health, private providers, specialists, and GPs. Such collaboration could refine DRG into a building block for a future National Health Insurance scheme. Ultimately, Budget 2026 must stabilise the workforce, decongest facilities through stronger public-private collaboration, and rebuild trust via transparent, inclusive governance—laying the foundation for universal health coverage and a resilient Malaysian health system.