A reseach publication by Polish authors Marzena Tambor, Jacek Klich, and Alicja Domagała titled “Financing Healthcare in Central and Eastern European Countries: How Far Are We from Universal Health Coverage?” explores how healthcare systems of Central and Eastern European countries underwent enormous transformation, resulting in departure from publicly financed healthcare after the fall of communism.
This had significant adverse effects on equity in healthcare, which are still evident, concluded authors.
In this paper, authors (health economists and health policy analysts) analyzed the role of government and households in financing healthcare in eight countries (EU-8): Czechia, Estonia, Hungary, Latvia, Lithuania, Poland, Slovakia, and Slovenia.
A desk research method was applied to collect quantitative data on healthcare expenditures and qualitative data on gaps in universal health coverage. A linear regression analysis was used to analyze a trend in health expenditure over the years 2000–2018.
Results indicate that a high reliance on out-of-pocket payments persists in many EU-8 countries, and only a few countries have shown a significant downward trend over time.
The gaps in universal coverage in the EU-8 countries are due to explicit rationing (a limited benefit package, patient cost sharing) and implicit mechanisms (wait times).
Latvia’s numbers in brief are:
- life expectancy at birth is 75.1 years (2018),
- population percentage claiming healthcare should be the government’s responsibility is 98% (2016),
- health expenditure as % of GDP is 6.21% (2018),
- domestic general government health expenditure as % of general government expenditure is 9.6% (2018),
- government/compulsory scheme expenditure as % of current health expenditure is 59.88% (2018),
- out-of-pocket health expenditure as % of current health expenditure is 39.18% (2018), down from 47.66% in 2000,
- % of Population Covered based on participation in insurance scheme – 100%.
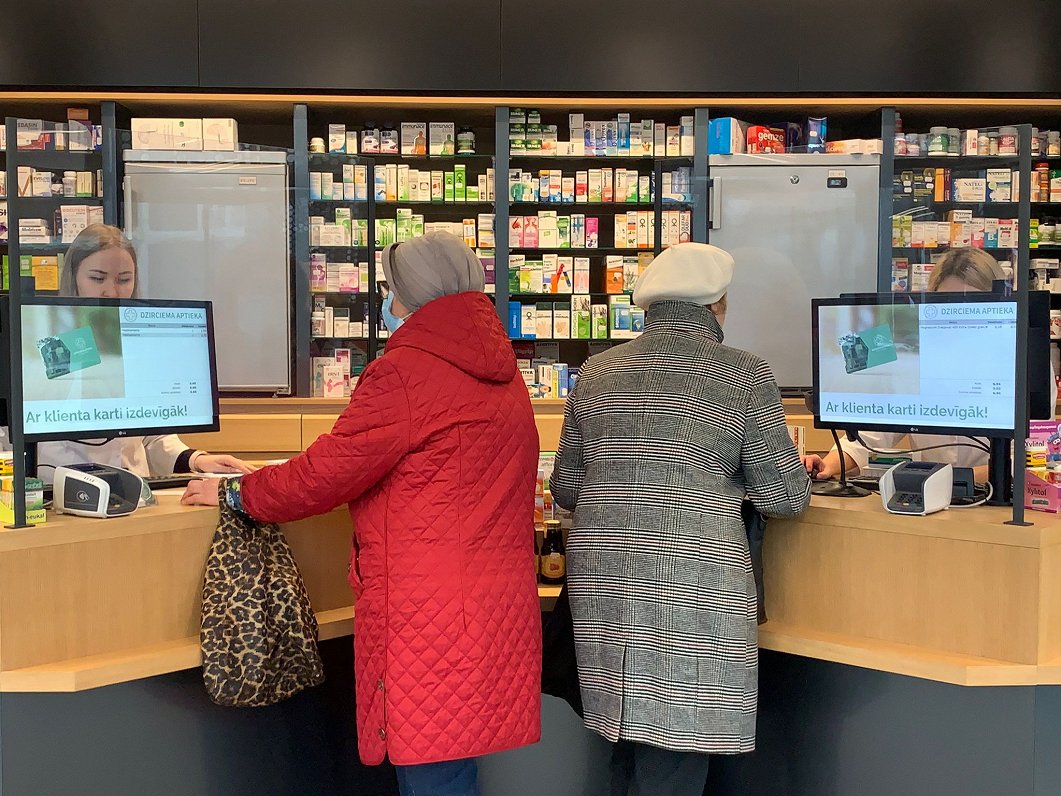
In terms of out-of-pocket payments, households in Latvia mostly contribute to financing medical products and therapeutic appliances (over 88%), dental care (over 80%), medicines (over 60%), as well as specialized outpatient curative care (almost 50%).
Between 2018 and 2019, a mandatory health insurance system was in place in Latvia. The full benefit package was available for individuals paying the insurance contribution and to those in one of 21 population groups covered by the state (e.g., children, pensioners). Others were granted access to a minimum benefit package financed by the state (emergency care, primary care, maternity care, psychiatric care, treatment of infectious diseases, and reimbursement of pharmaceuticals).
It is suggested that there is a need to increase the role of public financing in Central and Eastern European countries through budget prioritization, reducing patient co-payments for medical products and medicines, and extending the benefit package for these goods, as well as improving the quality of care.
Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7913209/