The now: removing financial barriers to COVID 19 testing and services
On May 1, the Kenyan Ministry of Health rolled out free testing for COVID 19 in Nairobi and other areas with disease hotspots. Two days later, the Ministry noted in dismay that the turnout for free testing was much lower than what they had hoped. The reason why the average Kenyan was not queuing up to get a free test was because he or she dreaded the prospect of mandatory quarantining at government designated sites. And a big part of that fear stemmed from having to pay for the quarantining. In the weeks preceding the free testing campaign, there had been news reports about people struggling to clear their bills even at public quarantine centers that were meant to be modestly priced and being held at the facility till they find the money. A leading daily paper released a video clip showing detainees scaling the wall to escape from one such facility.
On May 6, the Ministry announced that it was waiving all charges for quarantining. While this will not fix everything – folks who have experienced the quarantine facilities have also complained about unsanitary conditions and a lack of food – it is expected to a go a long way to encourage people to get tested. While this move serves the most immediate need for removing financial barriers to COVID 19 health services, the global pandemic has introduced uncertainty about the future of a much broader and comprehensive reform to enable all Kenyans to access the health services they need without fear of its financial costs.
The forever: improving financial access to healthcare on the path to Universal Health Coverage
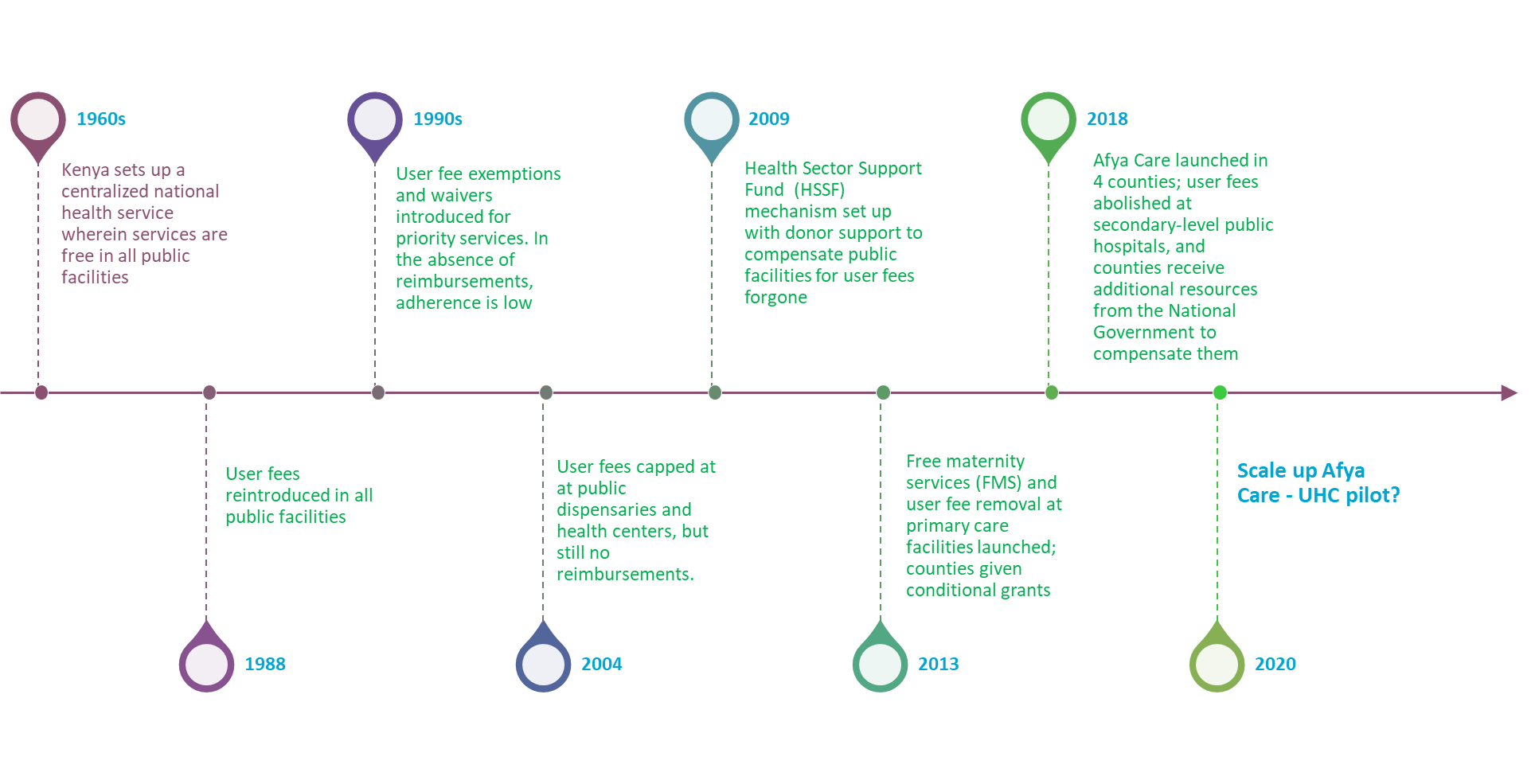
Before the pandemic broke, the National Government was poised to scale up the Afya Care universal health coverage (UHC) program, which it initiated in 4 counties in 2019. Under the pilot program, the 4 county governments agreed to discontinue all user charges at public sector hospitals. In its place, they received additional resources from the National Government in the form of medicines and non-pharmaceutical supplies as well as funds to cover the operating costs of public hospitals, invest in additional health infrastructure and health workers, and finance community health services. This program is an extension of a 2013 government policy that removed all user charges at primary care facilities and started reimbursing them for it (see figure that summarizes the history of user fee policies in Kenya).
Taken together, the 2013 policy and the 2018 UHC scheme – when scaled up — will allow Kenyans to access health services from all public facilities free of charge. There has been discussion of this model paving the way for a UHC fund that may eventually be managed by the National Hospital Insurance Fund and the creation of networks of care that include private providers. Such a transition would be a huge step in the right direction to remove financial barriers to access and increase financial risk protection. In a 2018 household health expenditure survey[1], a fifth of Kenyans cited the costs of seeking health services as a reason for foregoing care when they are ill. As many as 1.1 million individuals are pushed into poverty as a result of out-of-pocket spending on healthcare.
Before COVID-19 happened, the National Government was moving full steam ahead, signing agreements with counties to scale up the Afya Care program to the whole country. Now, for obvious reasons, all attention and government resources are focused on the pandemic; indeed some UHC funds have already been re-allocated to hiring more health workers. This is understandable and necessary. But even the National Government is moving rapidly to make COVID 19 testing and treatment available to everyone, the clock is being turned back in the UHC pilot counties. The pilot phase having ended, some of the counties are starting to charge patients for hospital visits. This seems particularly worrying given that the pandemic has delivered a heavy blow to the economy and Kenyans around the country – nearly 80% of whom are engaged in the informal sector and lack the option of working from home – are facing extreme economic hardship.
As Joe Kutzin and his colleagues wrote in a recent blog on health financing priorities in the age of COVID 19, “the choice is not between health security and UHC” and that investments in core health system functions solves for both. We urge Government of Kenya to stay the course on its UHC agenda, removing financial barriers to healthcare services, now and forever.
[1] Ministry of Health, Government of Kenya. 2018. Kenya Household Health Expenditure and Utilization Survey.Nairobi: Government of Kenya.
Nirmala Ravishankar (ThinkWell) and Edwine Barasa (KEMRI Wellcome Trust)

