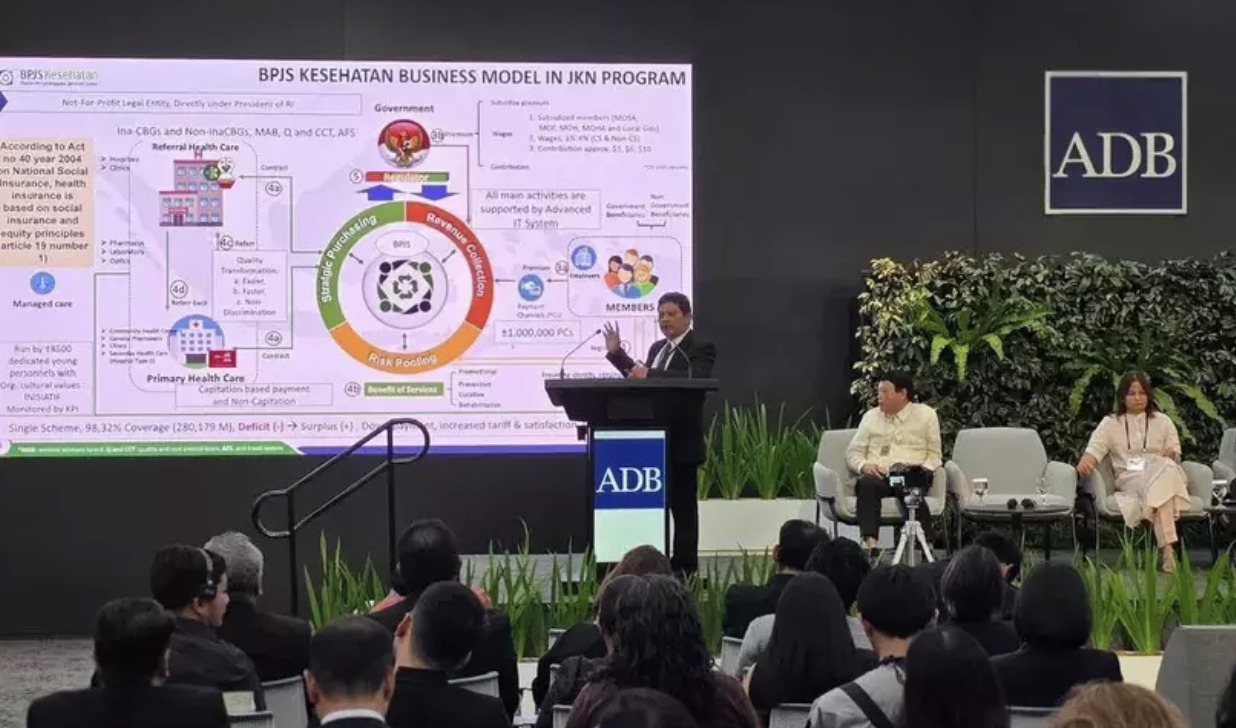
Indonesia has gradually extended social health protection to all Indonesian citizens. Achieving universal health coverage (UHC) is mandated under Law No. 40/2004 of the National Social Security System. However, the implementation was delayed for a decade. In 2014, Indonesia introduced a major health care reform advancing UHC by merging all fragmented health insurance schemes into a single universal scheme for all Indonesian citizens, the Jaminan Kesehatan Nasional (JKN)[1]. The financial contribution for low-income groups is subsidized by the government, and a mix of public and private providers delivers health service benefits. The JKN is one of the largest single payer schemes in the world. It is managed by the Badan Penyelenggara Jaminan Sosial (BPJS), which also administers Indonesia’s national insurance.
Financial protection is a key policy focus
Strengthening primary care for improving access to health care
Noncommunicable diseases (including stroke, heart disease, diabetes) are the leading causes of premature mortality and disability in Indonesia. There is broad consensus that prevention and early detection could mitigate the severity and progress of disease. The health system made a paradigm shift from curative to preventive-promotive services. It did so by strengthening and incentivizing primary health care services with supporting innovation and technology. This shift was reflected in payment mechanisms linked to performance of primary health care centers that boosted preventive and promotive services such as health examinations and screening. Performance-based capitation payment is used by the JKN for primary health care providers, with the aim of improving service provision and performance.
[1] Herawati, Franzone, R., Chrisnahutama, A. Universal Health Coverage: Tracking Indonesia’s Progress. Perkumpulan PRAKARSA: Jakarta; 2020.
[2] BPJS Kesehatan. JKN has revolutionized health services in 10 years: BPJS. Antara 2023 Jan 30 [cited 2023 Feb 5].
[3] World Bank Database. Out-of-pocket expenditure (% of current health expenditure) – Indonesia; 2019 [cited 2023 Feb 5].
[4] Haryati, S. Catastrophic spending in households with JKN declines to four percent. Antara. 2022 Dec 17 [cited 2023 Feb 5].